The word Lymphedema is derived from the words “lymph” (a fluid with a high protein concentration secreted by the lymphatic system) and the word “oedema” from the Greek οἴδημα meaning swelling. A limb affected by lymphedema will therefore be a limb “swollen with lymph”.
Lymphedema is a chronic condition that is becoming increasingly important in the scientific field due to the application of increasingly effective treatments. In fact, it is turning out to be no longer an unanswered pathology, but a field open to both different treatment options and major future developments.
What is lymphedema?
Lymphoedema is an oedema, i.e. an accumulation of fluid with a high interstitial protein concentration. It is due to a reduced transport capacity of the lymphatic circulation.
The increased protein concentration differentiates it from all other oedemas and is responsible for symptoms and signs that allow the classification of lymphedema into primary and secondary
Difference between oedema and lymphedema
Generally, oedema is defined as an abnormal accumulation of fluid that occurs in the body’s interstitial space (such as in the pericardial sac, intrapleural space, peritoneal cavity or joint capsules).
There are many causes of oedema, the most common of which include congestive heart failure, constrictive pericarditis, nephrotic syndromes, liver disease (cirrhosis), allergic reactions (urticaria or angioedema), malabsorption, caloric-protein malnutrition, obstructive sleep apnoea, pregnancy or side effects of medication. When unilateral or asymmetrical oedema is present, venous thrombosis is suspected.
Localised oedema is generally due to cellulitis, chronic venous insufficiency, deep vein thrombosis, lymphoedema or May-Thurner syndrome. When the oedematous area is warm and the patient’s vital parameters are unstable (febrile, tachycardic or tachypnoea), infectious and/or thrombotic causes must be suspected.
Primary and secondary lymphedema: differences
Primary (or congenital) lymphedema refers to lymphedema due to a defect, presumably genetic, in the lymphatic drainage, which is triggered by structural alterations in the lymphatic system. It is understood to be lymphatic oedema that is evident as early as the first months of life, in infancy or youth. It normally appears as a result of the condition already present at birth.
Secondary lymphedema refers to lymphedema that occurs as a result of external events that damage the lymphatic drainage pathways. Examples include the removal of lymph node stations following cancer surgery, degeneration of lymph node stations following radiotherapy, the presence of traumatic events and parasitosis (including filariasis).

How does the lymphatic system work
In our body there are two major systems responsible for transporting blood, the arterial and venous systems. The two systems converge at the periphery, where arterial and venous capillaries and the interstitium meet.
Arterial blood flows through the capillaries carrying nutrients to the tissues, while the venous system begins to collect waste substances.
The interstitium is made up of a network of cells and fibres and is the place where interstitial fluid, consisting of water, proteins, mineral salts and various types of cells, flows.
The lymphatic system is a drainage system parallel to the venous system and has the basic task of draining interstitial fluids within the peripheral connective tissue. If there is an increase in the production of interstitial fluid, the lymphatic system maintains the balance.
It is precisely when this does not happen that the condition known as “oedema” occurs.
Symptoms of lymphedema
Lymphedema generates characteristic symptoms including chronic swelling of the limbs, feeling of heaviness, tension and soreness of the affected limb.
It is a pathology that manifests itself asymmetrically. This means that it only affects one arm or one leg. Even in rare cases where it may affect both limbs, one limb tends to be more swollen than the other.
The swelling can be mild or severe, to the point of degenerating in some cases into elephantiasis, a disease characterised by abnormal thickening of the skin and underlying connective tissue.
These are not the only symptoms that can occur in a patient with lymphedema.
The other symptoms are almost all skin-related. In fact, as well as thickening, it becomes more fragile and more susceptible to infection. It is also easy to observe a change in colour, with the skin appearing shinier and at the same time discoloured.
In some cases, the affected person, in addition to the heaviness and constriction of the limb, may feel tension and itching of the skin.
This is why lymphedema can be bothersome despite not being a painful condition.
Lymphedema: The cause
Causes of lymphedema include:
Excluding primary lymphedema, which we recall is due to a malformation and thus a malfunction of the lymphatic vessels or lymph nodes, secondary lymphedema arises following surgery for tumour pathology with removal of lymph nodes.
Other causes of lymphedema are as follows:
- of parasitic origin
- related to chronic venous insufficiency of the lower limbs
- associated with systemic problems e.g. post-traumatic
- heart or liver conditions.
Diagnosis
The diagnosis of lymphedema is an indispensable procedure for defining the most correct treatment to be implemented.
Lymphedema is diagnosed predominantly clinically, i.e. by direct medical observation of the affected limb, although it may be supported by instrumental examinations that can confirm the diagnostic suspicion, such as ultrasound investigation, which can give a clear idea of the stage of the lymphedema.
The main advantage of the diagnosis of this disease is that it is characterised by the involvement of only one limb, which makes it easier to recognise it and distinguish it from other pathological conditions.
The areas that are mainly affected by lymphedema are the lower limbs (especially in the case of primary lymphedema) and upper limbs (especially after oncological surgery such as mastectomy)
The differential diagnosis, i.e. the one that attempts to exclude among various similar manifestations those that do not include the set of symptoms found during examinations, must be performed in the presence of oedema dependent on congestive heart failure, kidney failure and liver failure. In fact, these three diseases often have oedema among their symptoms and, although lymphedema is not directly fatal, if left untreated it can initiate a series of more serious pathologies, such as fibrosis
Therapies
For the treatment of lymphedema, the treatment options are varied. These include:
- Manual lymph drainage
- The pneumatic pressotherapy , which we will discuss in more detail in the following section
- Respiratory physiotherapy
- Hydrokinesiotherapy
- Diet
- Drug therapy
- Physical therapy (e.g. electrostimulation)
- Derivative microsurgery
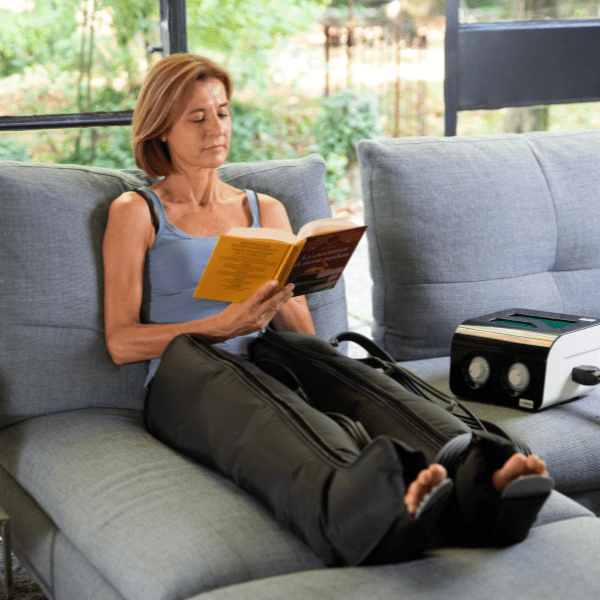
Specifically, pressure therapy promotes fluid displacement, leading to an increase in the speed of venous and lymphatic flow. This limits the processes of stagnation and retention, favouring the elimination of lymph. The resulting reduction in oedema relieves swelling and related pain.
Pressotherapy for lymphedema: does it work?
Let’s start with the bad news: there is, to date, no real cure that makes lymphedema disappear, but there are ways to relieve it.
In fact, under your doctor’s instructions, there are a number of procedures aimed at reducing swelling and promoting lymphatic drainage that we have outlined above, and pressotherapy is one of them. In fact, it has been shown to be absolutely effective in reducing oedema and, in general, in moving lymphatic stasis, but beware that it should not be considered a “monotherapy”!
As effective as pressotherapy for legs and arms can be, it should be combined with other practices such asmanual lymphatic drainage, lymphological bandages and the use of an elastic brace for better and longer-lasting results.
But which device to choose?
The best product should be versatile in compressing the affected area and easy to use since the treatment will have to be carried out every day:
for this reason the home pressotherapy can be a valuable ally!
I-Pressis our Made in Italy pneumatic pressotherapy! Easy and safe, it can be your main ally against lymphoedema in the legs and arms.
The operating principle is based on the possibility of exerting pressure that moves in waves from the bottom to the top (distal-proximal), in the treated area, with the use of special applicators built in sections that inflate in sequence. It is precisely the sequence of inflating and deflating the applicators (which, moreover, gives a pleasant and not at all painful sensation) that will generate fluid mobilisation and thus stimulate the beneficial effects!
All you have to do is find the right size of leggings, armbands and abdominal band for you and start your treatment in the peace and privacy of your own home!
Bibliography:
- Physiology, Edema
Daniella Lent-Schochet; Ishwarlal Jialal. https://europepmc.org - Mortimer PS, Rockson SG. New developments in clinical aspects of lymphatic disease.
- https://www.grupposandonato.it/news/2020/novembre/linfedema-sintomi-cause-trattamenti
- Brown-Dayan-Kataru-Mehrara. The Vicious Circle of Stasis, Inflammation, and Fibrosis in Lymphedema Plast Reconstr Surg. 2023 Feb 1; T





