Arthrosis is a chronic degenerative disease that affects the joints and cartilage tissue of hte bones.
The most affected joints are those on which the weight load is greatest, such as the hips, knees, and spine.
The symptoms of arthrosis
The symptoms of arthrosis are mainly pain, swelling and stiffness. They begin to occur around the age of fifty due to the deterioration of cartilage and the resulting rubbing of bones against each other. In particular, the frequency is higher in women after menopause.
In the case of people affected by the disease before the age of 50, however, there are no differences between men and women. The onset of symptoms, in fact, does not depend on hormonal changes but on working conditions and daily activities.
This condition can arise in a healthy joint for no clear reason or as a result of congenital deformity, trauma, infection, inflammation, or muscle overload.
Differences between arthrosis and arthritis
Before describing the condition, it is essential to emphasize the difference between arthritis and arthrosis, as confusion often arises.
Although they have some common features, arthritis is an inflammatory condition involving the joints, while arthrosis is a chronic degenerative noninflammatory form.
But how to tell if it is arthritis or arthrosis?
Arthritis often has symptoms such as pain, swelling and redness of the joints, which may be intermittent or persist over time.
In contrast, arthrosis generally causes joint pain and stiffness, especially after physical activity or upon awakening in the morning, with the presence of joint crepitus. In addition, while arthritis can strike at any age and can affect multiple joints at once, arthrosis develops gradually with age and tends to affect specific joints subject to greater wear and tear, such as the knees, hips, and hands.
Types of arthrosis
There are various forms of arthrosis, which differ from each other mainly according to the area of the body affected.
This involves the appearance of slightly different symptoms, but more importantly it involves the use of specific treatments and remedies.
Let’s take a look at them:
1. Cervical arthrosis
Cervical arthrosis affects the most mobile part of the spine. It affects both the surface of the vertebrae on the joint side and the cartilage discs between the vertebrae.
The causes of cervical arthrosis depend on an irregular lifestyle or poor posture and not only on aging. In fact, it is a form of arthrosis that can affect young people as well.
The main symptoms are manifested by a feeling of pain and stiffness in the neck and nape of the neck. Other possible symptoms include headaches and dizziness, as well as nausea, dizziness, and impaired vision or intolerance to noise. In addition, bony protuberances are created on the vertebrae, called osteophytes.
This type of arthrosis tends to worsen and spread to other areas, including the shoulders and fingers of the hands.
At present, it is not possible to recover completely from cervical arthritis.
However, the patient can rely on natural remedies such as massage and physical rehabilitation therapies or take pain-relieving and anti-inflammatory drugs to relieve symptoms. Myorelaxants can also have positive effects in the acute phase of the disease, but it is important to maintain a low dosage to avoid side effects.
If the nerve or spinal cord is compressed, then surgery may be necessary.
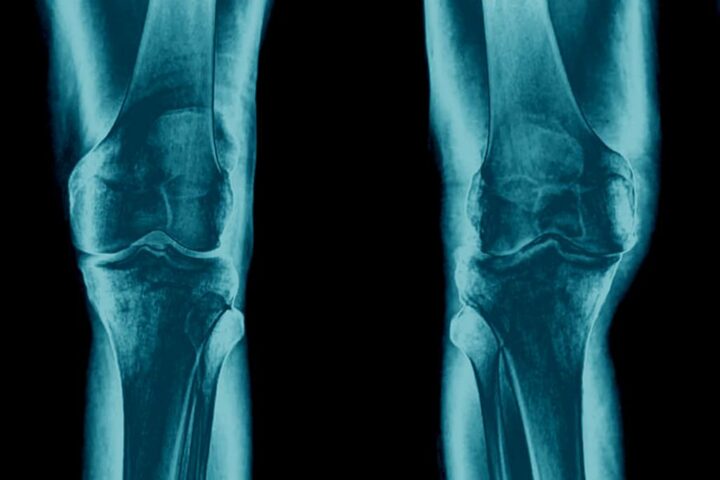
2. Arthrosis of the knee
Another type of arthrosis is that of the knee, a chronic inflammation due to degeneration of the cartilage layer present between the femur and tibia.
Major risk factors include age, obesity, and any previous surgeries such as meniscus removal surgery (meniscectomy).
The symptoms of knee arthrosis are always joint pain and stiffness, redness, swelling, creaking, and reduced mobility.
This form of the disease is also an irreversible condition. The only possible treatments are aimed at reducing pain and restoring some of the mobility of the knees.
3. Arthrosis of the hip.
Another form of this condition is arthrosis of the hip, also known as coxarthrosis. This is the inflammation of the cartilage that covers the hip joint.
Inflammation arises due to cartilage deterioration. Specifically, the affected layer of cartilage is that covering the upper end of the femur.
The symptoms are, again, pain and a reduced ability to move. The pain tends to be felt in the groin and in the front part of the leg. In the early stages of the disease it can be felt only by making certain movements, but over time it worsens and is felt even at rest.
Again, the patient may take pain-relieving and anti-inflammatory drugs with the sole purpose of relieving the pain and not to limit the damage to the joint.
4. Arthrosis in the hands
This is normally due to aging or a genetic predisposition, but it can also depend on trauma, fractures or infection.
The main symptoms include pain in the joints of the hand, swelling and tingling.
This type of arthrosis may be asymptomatic at first, but it tends to progress to the point of generating pain even at rest.

5. Interapophyseal arthrosis.
Interapophyseal arthrosis, also known as posterior vertebral arthrosis, affects the spine and particularly the zygapophyseal joints, which are the main joints of the back.
It involves erosion of the cartilage with which these joints are covered, reduced joint space, osteosclerosis, and osteophytosis.
Causes are determined by age, gender, genetic predisposition, sedentary lifestyle, and postural vices. For example, menopausal women tend to be more affected by the disease.
The main symptoms are stiffness and pain in the back, as well as increased difficulty in simple movements.
At present, this type of disease cannot be cured. Therapies, therefore, are aimed at keeping it under control and slowing down the process of cartilage degeneration.
Natural remedies may include performing targeted physical exercises and following a diet to lose weight.
Pain-relieving, anti-inflammatory, and muscle relaxant drugs, on the other hand, can serve to relieve pain.
6. Foot arthrosis
Arthrosis in the feet affects the cartilages of the joints of the bones of the foot.
The causes are those of other forms of arthrosis, to which are added the use of inappropriate shoes or excessively high heels.
Symptoms are also common ones of the disease. Since the joints affected are quite numerous, the symptoms can spread to various areas of the foot and make it almost impossible to walk.
As for treatment, again taking medication and performing physical exercises are only meant to relieve pain and slow down the degenerative process of cartilage.
7. Arthrosis of the shoulder
Shoulder arthrosis is characterized by its slow and gradual evolution.
The main causes include aging, but it can also be related to rheumatoid arthritis or a shoulder fracture.
As for treatment, some physical therapies can improve the patient’s condition. In addition, through arthroscopy, very small pieces of inflamed cartilage and tissue can be removed, at least partially reducing pain.
8. lumbar arthrosis
Lumbar arthrosis affects the vertebrae of the back and especially male individuals. It also has a higher incidence on elderly individuals.
Major causes include a sedentary lifestyle or, conversely, frequent performance of strenuous work. Any trauma or genetic predisposition to contract the disease may also be contributing factors.
In addition to the typical symptoms of arthrosis, in some more severe cases joint stiffness can lead to “locking” of the entire lower back. If the pain also affects the sciatic nerve, buttock and leg, it is called lumbosciatica. This implies that the discs present between the vertebrae are compromised.
Again, taking pain-relieving and anti-inflammatory drugs is prescribed to keep the disease under control and relieve pain.
9. Ankle arthrosis
Ankle arthrosis predominantly affects the elderly, but in others it may be a consequence of trauma, such as a fracture, or an obese condition.
The main symptoms are, as always, pain and joint stiffness but also swelling and unsteady feeling.
The main causes of arthrosis
We have already seen in previous paragraphs the triggers in different forms of arthrosis. So in this paragraph we will just summarize them.
Thus, the most common causes of arthrosis are:
- Age and aging.
- Genetic predisposition.
- A sedentary lifestyle that often results in weight gain.
- Wearisome activities performed daily, often in the work environment.
- Sports activities that can wear down the joints and cartilage of the feet, ankles, and knees.
- Fractures and joint injuries.
- Circulatory diseases that cause joint damage (e.g., hemophilia).
- Rheumatoid arthritis and other forms of arthritis that damage joints and, as a result, increase the chances of cartilage damage.
H3 Coffee is and arthrosis: is there a correlation?
The scientific evidence is not yet so well documented, in fact for now the correlation between coffee consumption and arthrosis has been explored in several studies, with mixed results. One study indicated that coffee consumption might increase the risk of arthrosis, especially of knee arthrosis, with the strongest association observed for decaffeinated coffee (1).
Another cross-sectional study of the Korean population found that consumption of more than 7 cups of coffee per day was associated with an increased prevalence of knee arthrosis in men, but not in women (2)
In short, there are no clear results yet, but we urge you to drink coffee in moderation.
The treatments for arthrosis.
As seen in the previous paragraphs, in most cases treatments for arthrosis have the sole purpose of relieving symptoms and slowing the deteriorating action on cartilage.
For treatment of arthrosis, our advice is first to consult your doctor, who will recommend the best approach, but generally the most common remedies include::
- Heat generation, such as through diathermy and ultrasound .
- Pain medications.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), for a limited period to avoid side effects.
- Myorelaxant drugs, to a lesser extent than painkillers.
How to prevent arthrosis
Before we talk about prevention, let’s try to understand what goes into worsening the condition In general of the risk factors that go into worsening arthrosis are sedentariness, being overweight, smoking and poor postural habits.
In addition, age, gender and genetic predisposition can also go to influence the onset and severity of arthrosis, but so what steps can be taken to prevent it?
- Don’t smoke Smoking is always a risk factor since it generally takes a toll on the body, reducing blood flow to the bones.
- Follow a diet to lose weight and place less burden on joints, particularly those of the hip and knees.
- Perform exercises to correct posture or scoliosis, strengthen supporting muscles, and recover mobility
- Warming up well/stretching is extremely important especially in more prone or older individuals who are about to exercise
Arthrosis, recommended therapies

Both magnetotherapy and ultrasound are particularly useful because they reduce pain and act in a very localized way on the area to be treated.
The antalgic action of pulsed electromagnetic fields works at the cellular level by reducing the degenerative action to joints and cartilage tissue.
Ultrasound (and thus ultrasound therapy) acts physically by micromassage to stimulate the mechanical part of the joint, increasing mobility, decreasing stiffness, and reducing the sensation of discomfort and pain.
Bibliography
- Coffee and the risk of osteoarthritis: a two-sample, two-step multivariable Mendelian randomization study (Zhang et al., 2024)
- Is knee osteoarthritis related to coffee drinking? A nationwide cross-sectional observational study (Bang et al., 2019)