What is headache
Headache is pain located inside the head or upper neck: it is the medical term for common headaches. It is a very common disorder, with varying intensity and duration, which can affect concentration, sleep quality and productivity. Early recognition of the type of headache helps to choose the most appropriate treatment and prevent recurrence.
The main categories of headache
To help you understand, it is useful to remember three main groups:
- Primary headaches
- Secondary headaches
- Cranial neuralgia, facial pain and other headaches
Primary headaches
These are the most common types and do not always have a single identifiable cause. There is often a genetic predisposition that interacts with environmental, hormonal or lifestyle factors.
Tension headache
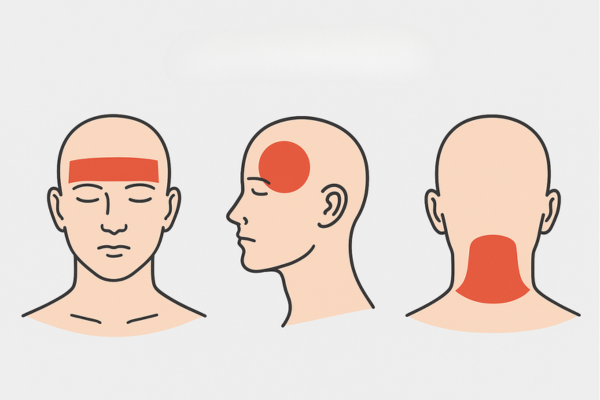
This is the most common type. The pain is mild to moderate but persistent, often felt as a band around the forehead, temples or back of the head. It is related to involuntary contraction of the neck and shoulder muscles and can be exacerbated by stress, anxiety, poor posture or visual overload. More common in women, it is classified as infrequent, frequent or chronic.
Migraine
More intense pain than tension headaches, in recurrent attacks lasting from 4 to 72 hours. Often associated with nausea, vomiting, photophobia, phonophobia and sometimes osmophobia. It mainly affects w s and can also occur in children. Triggers include hormonal imbalances, certain foods (aged cheeses, chocolate), lack of sleep, smoking and alcohol.
Cluster headache
Less frequent but more severe in intensity. Piercing, stabbing pain on one side of the head, with short, frequent attacks. It is often associated with tearing, drooping eyelids, runny nose or nasal congestion. Unlike migraine, nausea and vomiting are less common, but may occur. It mainly affects men and smokers; possible triggers include jet lag, stress and changes in sleep-wake patterns.
Secondary headaches
In this case, the headache is a symptom of another condition (e.g. infection, trauma, vascular or metabolic disorders). Management involves diagnosis and treatment of the underlying condition.
Ophthalmic headache
This is characterised by visual and neurological disorders: photophobia, seeing spots or flashes, increased tearing and temporary loss of vision. In forms with visual aura, an eye examination is useful to correct refractive errors such as myopia or astigmatism, which may contribute to the discomfort. However, the direct link between visual defects and headache has not been fully proven.
Cranial neuralgia, facial pain and other headaches
These result from inflammation or irritation of the cranial or cervical nerves and can be very painful.
Stabbing headache
A rare form, with episodes of acute, short-lived pain (‘thuds’ or ‘stabs’) that may recur over time. Medical evaluation is necessary to rule out secondary causes.
Clinical diagnosis process
The diagnosis starts with a thorough medical history of the location, intensity, duration and frequency of the pain, triggering factors, medications taken and associated symptoms. In the presence of “red flags” or atypical symptoms, tests such as CT/MRI, CT/MRI angiography, lumbar puncture, EEG in children, blood tests and spinal X-rays are used.
Headache symptoms
- Tension headache: diffuse and continuous pain, often in the front and back of the head.
- Migraine: severe, throbbing headache, unilateral or bilateral, with hypersensitivity to light and sound, nausea or vomiting.
- Cluster headache: very intense unilateral pain, with autonomic signs (red eye, tearing, blocked nose).
- Ophthalmic headache: visual aura and transient, reversible eye disorders.
The most common causes
- Tension: stress, anxiety, depression, poor posture.
- Migraine: neurovascular basis, hormonal, dietary and behavioural triggers.
- Cluster: possible hypothalamic/circadian alterations; triggers such as jet lag and alcohol.
- Ophthalmic: genetic/vascular components and pre-existing visual problems.
Treatments and prevention
Preventive therapy
For tension headaches: regular sleep, stress management, workplace ergonomics and moderate physical activity.
For migraine: prophylactic drugs (beta-blockers, antiepileptics, antidepressants) on medical advice. Some studies are exploring magnesium and B12, but evidence is limited.
For cluster headaches: pharmacological prophylaxis only under specialist supervision.
Symptomatic therapy

- Tension headaches and migraines: analgesics (paracetamol) and NSAIDs (ibuprofen); opioids/barbiturates not recommended.
- Cluster headache: 100% oxygen with a non-rebreather mask at 7–15 L/min for 15–20 minutes according to specialist advice.
- Home physical therapies:
- TENS: may be beneficial in some patients in reducing pain and muscle tension.
- Magnetic therapy: studied but with limited evidence; can be used as a support under medical supervision, with certified devices such as those from I-Tech Medical Division.





